Introduction: Navigating the Mysterious Realm of Adhesive Capsulitis
Adhesive capsulitis, commonly known as frozen shoulder, can be an incredibly perplexing and painful condition that significantly restricts shoulder movement. This comprehensive guide aims to shed light on this ailment, providing valuable insights into its causes, symptoms, diagnosis, treatment options, and preventive measures. Whether you’re personally dealing with frozen shoulder or seeking to enhance your understanding of musculoskeletal health, this guide will equip you with the knowledge to tackle adhesive capsulitis head-on.
Section 1: Anatomy of the Shoulder Joint and Capsule
To comprehend adhesive capsulitis, it’s imperative to grasp the intricacies of the shoulder joint and its surrounding structures. The shoulder joint, a ball-and-socket joint, offers an impressive range of motion but is inherently susceptible to various conditions. The joint is enclosed by a capsule—a fibrous structure that envelops and stabilizes it. When this capsule becomes inflamed and thickened, it results in the characteristic stiffness and pain associated with adhesive capsulitis.
The shoulder is a complex and highly mobile joint that allows for a wide range of motion in the upper extremity. It is made up of several bones, muscles, ligaments, and tendons. The primary bones and structures that make up the anatomy of the shoulder include:
- Humerus: The upper arm bone, which connects to the scapula and forms the ball-and-socket joint of the shoulder.
- Scapula (Shoulder Blade): A flat, triangular bone that forms the back part of the shoulder. It has several important features, including the acromion, coracoid process, and glenoid cavity.
- Clavicle (Collarbone): A long, slender bone that connects the sternum (breastbone) to the acromion of the scapula, helping to stabilize the shoulder joint.
- Glenoid Cavity: The shallow, socket-like portion of the scapula that forms the “socket” of the ball-and-socket shoulder joint. It articulates with the head of the humerus.
- Acromion: A bony projection of the scapula that forms the roof of the shoulder joint and articulates with the clavicle.
- Coracoid Process: A smaller bony projection of the scapula located in front of the acromion and provides attachment points for various muscles and ligaments.
The shoulder is surrounded by a network of muscles, tendons, and ligaments that help provide stability and enable its wide range of motion. Some of the key muscles of the shoulder include:
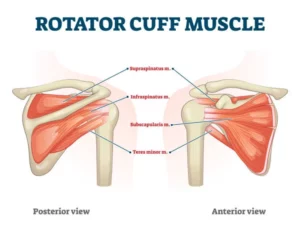
- Rotator Cuff Muscles: These four muscles (supraspinatus, infraspinatus, teres minor, and subscapularis) work together to stabilize the shoulder joint and facilitate various movements.
- Deltoid Muscle: The deltoid muscle covers the shoulder joint and is responsible for lifting and rotating the arm.
- Trapezius Muscle: This large muscle in the upper back and neck helps control the movement of the scapula and is involved in shoulder and neck movements.
- Pectoralis Major and Minor Muscles: These chest muscles are connected to the shoulder and play a role in movements like arm flexion and adduction.
The shoulder joint is further supported by several ligaments, including the coracoclavicular ligament, acromioclavicular ligament, and the glenohumeral ligaments.
In addition to these structures, there are bursae (small fluid-filled sacs) that help reduce friction between tendons, muscles, and bones in the shoulder, aiding in smooth movement.
Section 2: Unravelling the Causes
While the precise triggers of adhesive capsulitis remain somewhat elusive, certain factors are commonly associated with its development. Individuals with diabetes, for instance, are at a higher risk of developing frozen shoulder due to underlying metabolic and hormonal factors. Additionally, previous shoulder injuries, prolonged immobilization, and certain autoimmune conditions may contribute to the onset of this condition.
Section 3: Deciphering the Stages of Frozen Shoulder
Adhesive capsulitis typically progresses through three distinct stages: the freezing stage, the frozen stage, and the thawing stage. During the freezing stage, individuals experience a gradual increase in pain and stiffness, limiting their shoulder’s range of motion. This is followed by the frozen stage, characterized by persistent stiffness but diminished pain. Finally, the thawing stage sees a gradual return of shoulder mobility.
Section 4: Recognizing the Tell tale Symptoms
Early recognition of adhesive capsulitis symptoms is crucial for initiating timely treatment. Individuals with frozen shoulder may experience pain during both active and passive shoulder movements, accompanied by a noticeable reduction in range of motion. Everyday tasks such as reaching for objects or fastening clothing can become challenging and painful.
Section 5: Seeking Diagnosis and Medical Evaluation
A medical professional’s expertise is essential for an accurate diagnosis of adhesive capsulitis. Physical examinations, combined with a review of medical history, aid in ruling out other potential causes of shoulder pain and stiffness. Imaging techniques like X-rays and MRI scans can provide valuable insights into the severity of the condition and aid in developing an effective treatment plan.
Section 6: Crafting a Treatment Strategy
The treatment approach for adhesive capsulitis often entails a combination of therapies. Physical therapy plays a pivotal role in maintaining and gradually improving shoulder mobility. Therapists guide patients through specialized exercises that focus on stretching and strengthening the shoulder muscles. In cases of intense pain, nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroid injections may be prescribed to alleviate discomfort and reduce inflammation.
Section 7: Exploring Invasive Interventions
While most cases of adhesive capsulitis can be managed non-surgically, surgical interventions might be considered for severe and refractory cases. Procedures like manipulation under anaesthesia and arthroscopic release involve manipulating or removing the thickened capsule to restore range of motion. These interventions are typically reserved for cases where conservative treatments have proven ineffective.
Section 8: Embracing Preventive Measures
Prevention is a key aspect of musculoskeletal health, and understanding how to reduce the risk of developing adhesive capsulitis is paramount. Maintaining a consistent exercise routine that emphasizes shoulder mobility and strength is crucial. Avoiding prolonged immobilization and seeking early intervention for any shoulder injuries can also play a pivotal role in preventing the onset of frozen shoulder.
Section 9: Patience and Persistence in Recovery
Recovery from adhesive capsulitis is a journey that requires dedication and patience. It’s important to recognize that progress may be gradual, particularly during the thawing stage. Adhering to the prescribed treatment plan, regularly performing recommended exercises, and maintaining an open line of communication with healthcare professionals are essential steps on the road to full shoulder recovery.
Conclusion: Unfreezing the Potential of Adhesive Capsulitis
While adhesive capsulitis might present a formidable challenge, understanding its nuances empowers individuals to navigate the frozen shoulder journey with confidence. Through proactive measures, informed decisions, and diligent adherence to treatment plans, the frozen grip of adhesive capsulitis can be thawed, allowing individuals to regain their shoulder mobility and embrace an active and pain-free life.
We at All Out Physiotherapy we have near a decades worth of experience and with our proven framework of rehabilitation we are able to get down to the root cause of the problem and help you recover and achieve your goals.